Opioid Treatment Medication Choice Calculator
Help me choose
Answer a few questions to see which medication might be a better fit for your situation. This calculator is based on clinical evidence from the article about methadone and buprenorphine side effects in opioid use disorder treatment.
Methadone may be a better fit for you
Based on your responses, methadone may be the better treatment option for your situation. Methadone is particularly effective for heavy users and those who have been using opioids for many years.
However, it's important to know that methadone requires close medical supervision. It can cause drowsiness, constipation, and other side effects, but it's often the most effective treatment for long-term recovery.
Remember: If you're on methadone, follow your doctor's instructions closely. Never mix it with alcohol, benzodiazepines, or sleep aids. Your safety is the top priority.
Buprenorphine may be a better fit for you
Based on your responses, buprenorphine may be the better treatment option for your situation. Buprenorphine is safer for many patients and can be prescribed by your regular doctor rather than in a specialized clinic.
However, it might not be strong enough for heavy users. Some patients with long-term opioid use experience breakthrough cravings with buprenorphine.
Important: If you choose buprenorphine, be sure to take it correctly under your tongue. Swallowing it significantly reduces effectiveness.
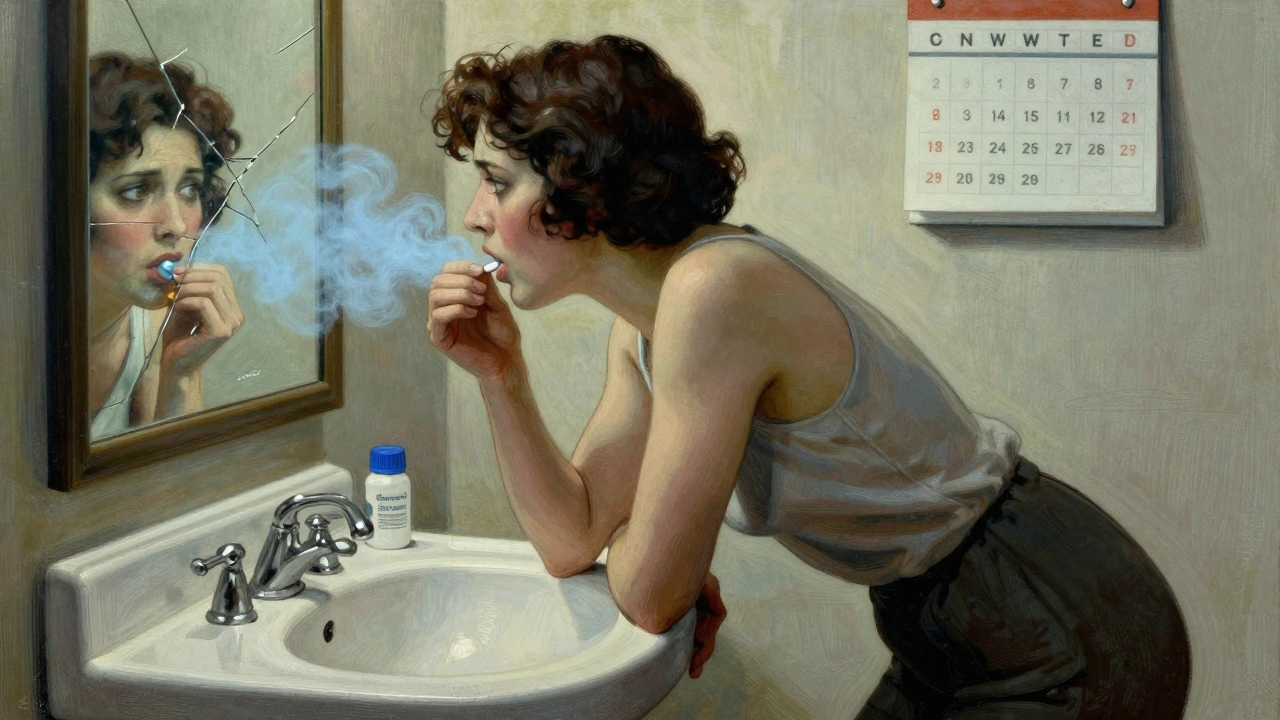
When someone is fighting opioid use disorder, methadone and buprenorphine can be life-saving. But they’re not without their own set of challenges. Many people start these medications hoping to feel normal again - to stop craving heroin or fentanyl, to hold a job, to be present for their kids. What they don’t always expect is how the treatment itself can change how they feel day to day. The side effects of methadone and buprenorphine aren’t just minor annoyances. They can shape whether someone stays in treatment - or walks away.
What methadone does to your body
Methadone is a full opioid agonist. That means it fully activates the same brain receptors as heroin or fentanyl, but in a slower, steadier way. This keeps cravings down and withdrawal at bay. But because it’s so strong, the side effects can be intense.
Most people on methadone report feeling drowsy, especially in the first few weeks. One patient in Bristol told me, “I’d sit at my desk and just zone out. My boss thought I was lazy. I wasn’t - I was just tired all the time.” Sleepiness affects nearly 1 in 3 people. Nausea and vomiting hit about 1 in 4, and constipation? That’s almost universal. One study found 40% of long-term users needed daily laxatives just to go to the bathroom.
But the real dangers are quieter. Methadone can stretch out the heart’s electrical cycle - known as QTc prolongation. At doses over 100mg a day, this happens in up to 35% of people. It doesn’t cause symptoms right away. But it can lead to sudden, fatal heart rhythms. That’s why doctors recommend an EKG before starting and again after a few weeks, especially if you’re on a higher dose.
Sexual problems are another hidden burden. About 3 in 10 men on methadone experience erectile dysfunction. Women report lower libido and irregular periods. These aren’t talked about enough in clinics. Many patients feel ashamed and stop asking for help - which means they stop coming back.
And then there’s the overdose risk. Methadone builds up in your system over days. If you take too much too fast - or mix it with alcohol, sleeping pills, or anxiety meds - your breathing can slow to a stop. That’s why methadone is only given in special clinics, with daily supervision at first. It’s safe… if you follow the rules. But if you don’t, the risk is real.
How buprenorphine is different
Buprenorphine, especially in the form of Suboxone (which includes naloxone), works differently. It’s a partial agonist - it activates opioid receptors, but only partly. That’s why it has a ceiling effect: after a certain dose, it doesn’t get stronger. That’s also why it’s much safer.
The most common side effects? Headaches. Up to 4 in 10 people get them. Then there’s mouth issues. Because Suboxone dissolves under the tongue, it can cause numbness, soreness, or a weird taste. Some patients say it feels like their tongue is wrapped in plastic. That’s not fun, but it’s not dangerous.
One big complaint? It doesn’t always work well enough. People with high opioid tolerance - especially those who used fentanyl regularly - often say buprenorphine doesn’t fully stop their cravings. A Reddit user wrote: “I took 24mg of Suboxone a day and still found myself buying pills on the street. It kept me from overdosing, but I was still chasing the high.” That’s not rare. Around 1 in 3 people on buprenorphine report breakthrough cravings.
But here’s the trade-off: because of that ceiling effect, buprenorphine is far less likely to cause fatal overdose. Even if someone takes too much, their breathing doesn’t shut down the way it can with methadone. That’s why it’s now the go-to for most new patients. You can get it from your regular doctor, not just a clinic. It’s easier to access. But access doesn’t always mean it’s the right fit.
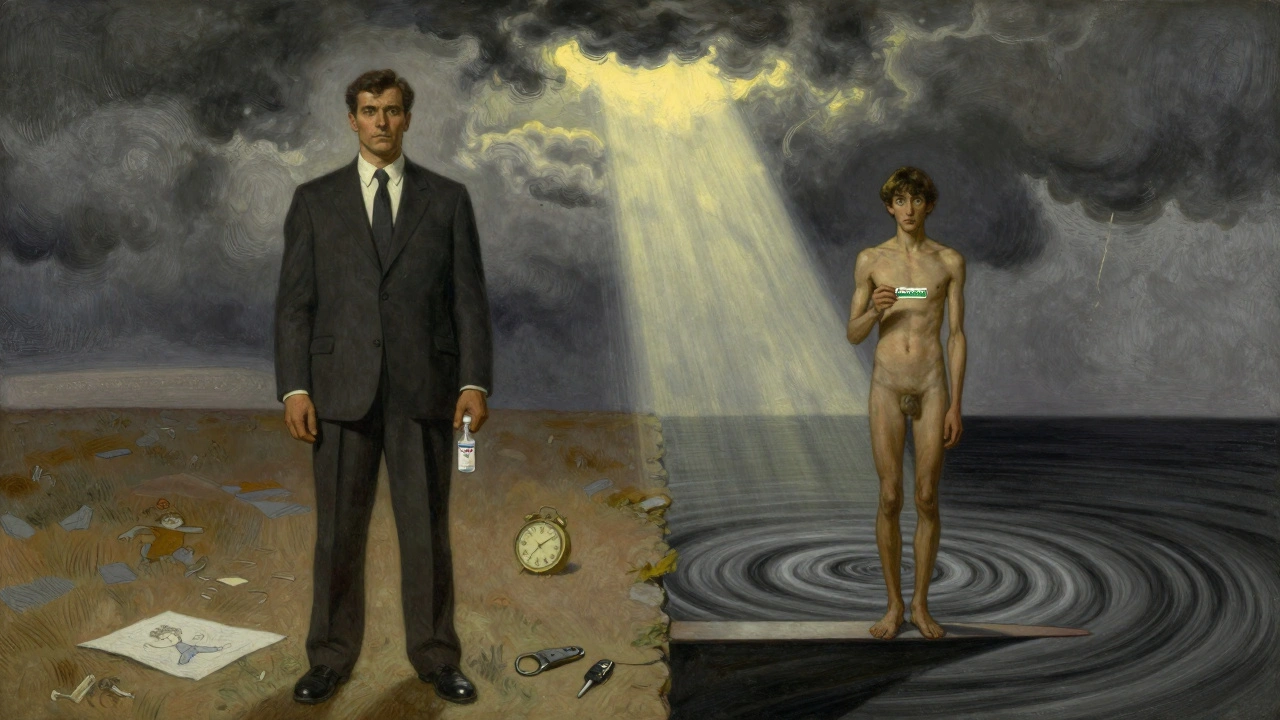
Which one is safer? It depends
It’s tempting to say buprenorphine is better because it’s safer. But that’s not the whole story.
Methadone keeps more people in treatment. In a 2024 study, 81.5% of people stayed on methadone after two years. Only 11.2% stayed on buprenorphine - the rest dropped out. Why? Because methadone works better for heavy users. If you’ve been using opioids for years, especially fentanyl, methadone often gives you the level of relief buprenorphine can’t match.
But if you’re newer to opioid use, or you’re worried about heart problems, or you live alone and don’t have someone to watch you take your dose - buprenorphine is the clear winner. It’s harder to overdose on. It doesn’t cause as much drowsiness. You can drive. You can work.
And here’s something no one talks about enough: the way you take the medication matters. Methadone is swallowed. Buprenorphine has to dissolve under your tongue. If you swallow it, you get almost none of the dose. That’s why some people feel like it’s not working - they’re not taking it right. A study found up to 60% of patients who thought Suboxone wasn’t helping were actually swallowing it instead of letting it dissolve.
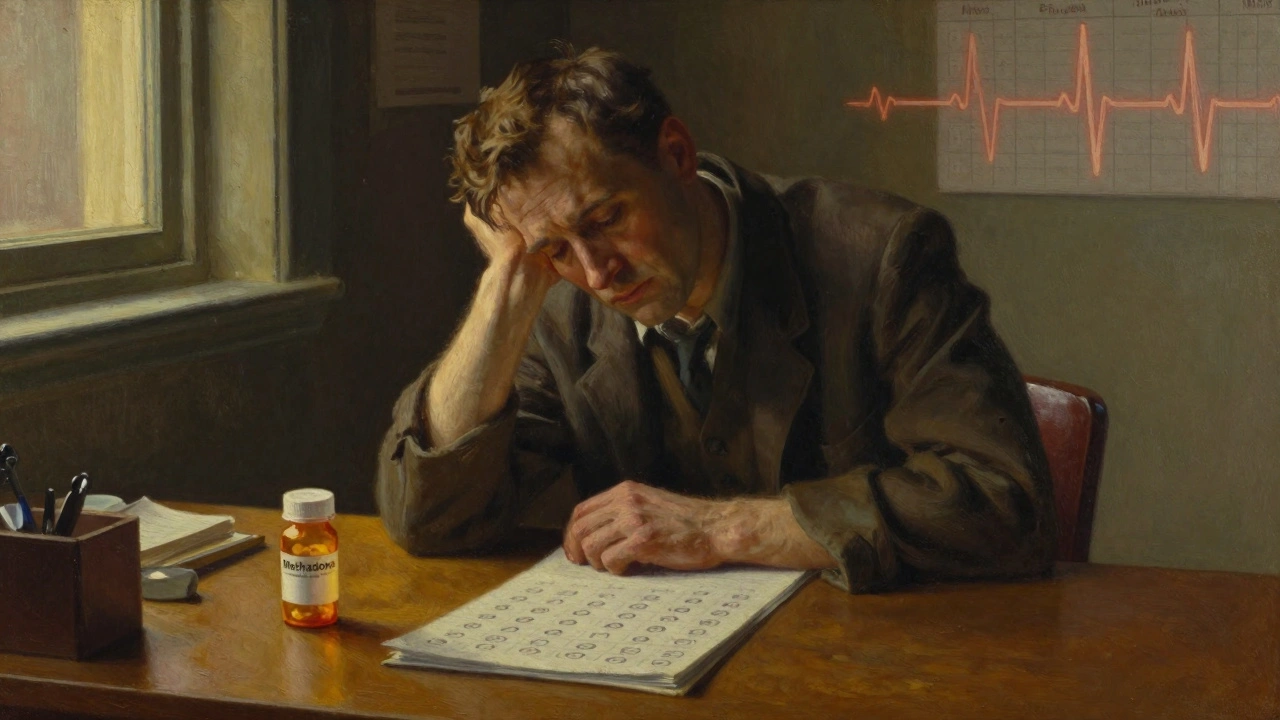
What no one tells you about long-term use
People think once you’re stable, the side effects fade. That’s partly true. But some stick around.
Long-term methadone users often develop hormonal changes. Low testosterone in men. Irregular cycles in women. That can lead to fatigue, weight gain, and depression - which makes it harder to stay motivated in recovery.
For buprenorphine, the biggest long-term issue is the ceiling effect. If your dose maxes out at 16mg and you still crave opioids, you’re stuck. You might not be overdosing, but you’re not fully free, either. Some patients say they feel like they’re just managing, not healing.
And then there’s the mental toll. Both drugs can cause memory problems and trouble focusing. Methadone users show bigger deficits in visual memory and attention - especially when driving. One study found methadone patients were twice as likely to have minor car accidents as people not on medication.
But here’s the surprising part: people who stay on methadone long-term often report higher satisfaction with their treatment. Even with the side effects, they say they feel more normal. More stable. More like themselves. Buprenorphine users, while safer, often say they feel like they’re holding on by a thread.
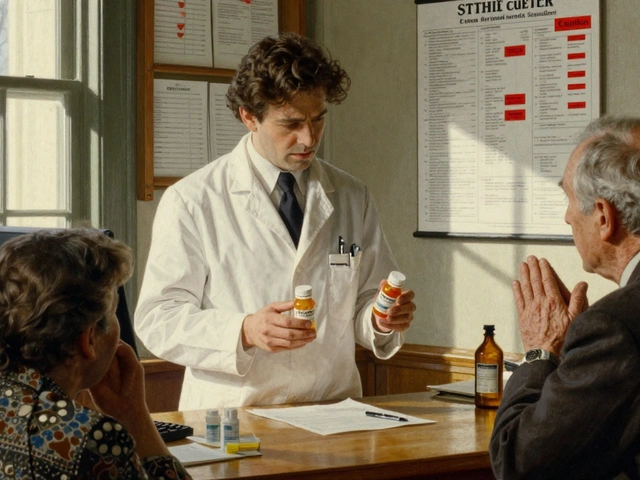
What to do if side effects are too much
Side effects don’t mean you have to quit. They mean you need to talk to your provider.
If you’re on methadone and you’re always sleepy, ask about your dose. Maybe you’re on too much. Maybe you need to wait longer between increases. If your heart is a concern, get an EKG. If constipation is ruining your life, ask for stool softeners or a bowel program. Don’t suffer in silence.
If buprenorphine isn’t stopping your cravings, don’t assume it’s your fault. Tell your doctor. You might need a higher dose - up to 24mg or more. Or you might need to switch to methadone. Or try the monthly injection, Sublocade. It avoids mouth issues and gives steady levels. But it can hurt at the injection site.
And never, ever mix either medication with alcohol, benzodiazepines, or sleep aids. That’s how people die. Even if you’ve been on it for months, the risk doesn’t go away.
Also, make sure you’re getting counseling. Methadone clinics usually require it. Buprenorphine providers? Not always. But therapy helps you understand why you used opioids in the first place. It helps you cope with the side effects without going back to street drugs.
The bottom line
Methadone and buprenorphine aren’t perfect. But they’re the best tools we have. Neither is a cure. But both can give you back your life - if you can manage the side effects.
Methadone works better for heavy users. It’s more likely to keep you in treatment. But it’s riskier. You need monitoring. You need patience. You need to accept that you might feel sluggish, constipated, or sexually impaired.
Buprenorphine is safer, easier to get, and less sedating. But it might not be strong enough. You might still crave. You might still feel like you’re on the edge.
The right choice isn’t about which drug is ‘better.’ It’s about which one fits your life, your history, your body, and your goals. And that’s something only you and your doctor can figure out - together.




Isabelle Bujold
Methadone’s QTc prolongation is way under-discussed. I’ve seen three patients in my clinic develop torsades de pointes after being on it for 6 months with no EKG follow-up. It’s not just about dose-it’s about baseline electrolytes, polypharmacy, and genetic factors like CYP3A4 metabolism. Most prescribers don’t check CYP450 panels. That’s negligence disguised as protocol. And don’t get me started on how clinics ignore the hormonal cascade-low testosterone isn’t just ‘a side effect,’ it’s a metabolic disruption that tanks motivation and muscle mass. Patients aren’t lazy-they’re biochemically depleted.
And buprenorphine’s ceiling effect? It’s a myth that it’s ‘safer’ for everyone. If you’re a 200-pound guy who used to shoot fentanyl daily, 16mg is like giving a firehose to someone with a thimble. You’re not treating addiction-you’re managing withdrawal symptoms while leaving the craving engine running. That’s why dropout rates are so high. We need tiered dosing protocols, not one-size-fits-all guidelines.
Also, nobody talks about the oral absorption issue with Suboxone. I had a patient who was swallowing it because she thought it was ‘faster.’ She didn’t know the naloxone doesn’t activate unless injected. She was getting 20% of her dose. We switched her to Sublocade and her cravings dropped 80% in two weeks. Education isn’t optional-it’s the first line of treatment.
Jordan Wall
OMG this post is SOOOOO deep 😍👏 I literally cried reading about the QTc thing-like, WHO KNEW??? 🤯 Methadone is basically a slow-mo cardiac grenade 💣 and buprenorphine is just… meh? Like, if you’re not getting 24mg you’re basically just ‘in recovery’ but still a zombie 🧟♂️ #PharmaIsLying #SuboxoneIsAScam
Also, did you know the FDA is hiding data because Big Pharma pays them? 🤫 I read it on a blog by a guy who used to work at Purdue. They’re all in cahoots. I’ve been on 32mg of Suboxone and still crave-so obviously it’s a plot. #WakeUpSheeple
Martyn Stuart
Let’s be clear: methadone and buprenorphine aren’t ‘alternatives’-they’re different tools for different clinical profiles. The key isn’t which drug is ‘better,’ but which pharmacokinetic profile matches the patient’s opioid tolerance, hepatic metabolism, and psychosocial stability. Methadone’s long half-life and full agonist activity make it superior for high-tolerance populations, particularly those with polysubstance use or chronic relapse patterns. Buprenorphine’s partial agonism and ceiling effect reduce overdose risk but compromise efficacy in severe cases.
Additionally, the absorption issue with sublingual buprenorphine is not anecdotal-it’s well-documented in pharmacokinetic studies. Swallowing it results in near-zero bioavailability due to first-pass metabolism. Clinicians must verify administration technique via direct observation or salivary testing. Without this, treatment failure is inevitable.
And yes, hormonal suppression is real. Both drugs suppress the HPG axis. Testosterone replacement therapy should be considered routinely in male patients on long-term MAT. This isn’t ‘side effect management’-it’s standard endocrine care. We’re treating a neuroendocrine disorder, not just addiction.
Chase Brittingham
I’ve been on methadone for 7 years. I’m not ‘fixed’-but I’m alive. I see my daughter every weekend. I work as a mechanic. I don’t lie awake terrified of withdrawal anymore. Yeah, I’m tired. Yeah, I need laxatives. Yeah, my libido’s gone. But I’m here. And I’m not ashamed.
People think if you’re on meds, you’re not ‘really sober.’ But sobriety isn’t about being drug-free. It’s about being free from the fear, the chaos, the needle in your arm. I’m not perfect. But I’m present. And that’s worth more than any ‘clean’ urine test.
Ollie Newland
That 81.5% retention rate for methadone vs. 11.2% for buprenorphine? That’s not a fluke. It’s biology. If your opioid tolerance is above 120mg morphine equivalent daily, buprenorphine’s ceiling is like trying to fill a swimming pool with a teapot. You’ll get wet, but you won’t be submerged.
And the sexual side effects? Yeah, they’re brutal. I didn’t tell my doctor for a year because I thought it was ‘normal.’ Turns out, testosterone levels dropped 60%. I started TRT and my energy came back. No one talks about this because it’s ‘embarrassing.’ But if you’re not talking about it, you’re not treating the whole person.
Dematteo Lasonya
I was on Suboxone for 9 months. Swallowed it by accident. Thought it wasn't working. Switched to methadone. Life changed.
Karl Barrett
There’s a philosophical layer here we ignore. Addiction isn’t just a biological disorder-it’s a rupture in identity. Methadone gives you back your body, but not your self. Buprenorphine gives you back your autonomy, but not your peace. The real question isn’t ‘which drug works better?’ It’s ‘which version of yourself are you trying to become?’
Some people want to be free of craving. Others want to be free of shame. Methadone patients often say they feel ‘normal’-not euphoric, not numb, just… human. Buprenorphine users say they feel ‘managed.’ One is restoration. The other is containment.
And therapy? It’s not an add-on. It’s the scaffold. Without it, you’re just trading one dependency for another. Medication is the bridge. Therapy is the reason you cross it.
Jake Deeds
Let’s be honest-methadone clinics are basically prison for people who used to be addicts. You have to show up every day. You get watched. You’re treated like a criminal. Meanwhile, buprenorphine? You get a script like a diabetic. Why? Because rich people get safer drugs. Poor people get the one that makes them sleepy and constipated.
And don’t even get me started on the ‘dose titration’ nonsense. You think your doctor actually cares if you’re tired? Nah. They’re just trying to hit their quota. If you’re still craving, they’ll say ‘you need more willpower.’ Meanwhile, they’re cashing their paycheck.
This isn’t medicine. It’s social control dressed in white coats.
val kendra
YOU CAN DO THIS. I was on methadone for 5 years. Got off. Now I’m clean and running marathons. Side effects suck, but they’re temporary. Your brain heals. Your body heals. Don’t give up because you feel sluggish. That’s your body rewiring. Keep going. You’re not broken-you’re becoming.
And if you’re on Suboxone and it’s not working? ASK FOR MORE. Don’t be shy. 24mg isn’t too much. It’s what your brain needs. And if your doctor says no? Find a new one. You deserve better.
Also-drink water. Eat fiber. Move your body. These aren’t ‘hacks’-they’re survival tools. You’re not just fighting addiction. You’re rebuilding your life. One day at a time.
Ben Choy
Just wanted to say thank you for writing this. I’ve been on buprenorphine for 3 years. I still get headaches. My tongue still feels weird. But I’ve held the same job. I’ve watched my nephew grow up. I didn’t OD. That’s a win.
I used to think I was weak for needing help. Now I know: needing help isn’t weakness. Staying silent is.
And if you’re reading this and you’re scared to talk to your doctor? Just say ‘I’m still craving.’ That’s all you need to say. They’ll listen. I promise.
Emmanuel Peter
Let’s cut the BS. Methadone is just a legal opioid with more side effects. You’re not ‘in recovery’-you’re just replacing one drug with another. And buprenorphine? It’s a placebo for people who can’t handle withdrawal. The whole MAT system is a scam to keep people dependent on pills forever.
Real recovery means going cold turkey. No meds. No excuses. If you can’t do that, you’re not ready. Stop blaming the drugs. Blame yourself.
Ashley Elliott
I’ve been a nurse in an addiction clinic for 12 years. I’ve seen people on methadone who go from homeless to holding a job. I’ve seen people on buprenorphine who finally sleep through the night. Neither is perfect. But both save lives.
The real tragedy? People don’t get the dose they need because of stigma. Or because insurance won’t cover it. Or because their doctor thinks ‘24mg is too much.’
Don’t let anyone make you feel guilty for needing help. You’re not weak. You’re brave.
Augusta Barlow
Did you know methadone is used in CIA mind control experiments? The QTc prolongation? That’s not a side effect-that’s a tracking mechanism. They want you dependent so they can monitor your heart rhythm remotely. And buprenorphine? The naloxone is a trigger. If you ever try to go off it, they activate the withdrawal. That’s why you can’t quit.
Big Pharma owns the FDA. The CDC. The WHO. Even your doctor. They’re not helping you-they’re keeping you in the system. You’re a product. Your addiction is their revenue stream.
And if you think this post is ‘educational,’ you’ve been programmed. Look at the language. ‘Stable.’ ‘Treatment.’ ‘Compliance.’ That’s not medicine. That’s control.
Rachel Bonaparte
Oh please. Methadone is a government-approved opioid trap. You think your doctor cares if you live? They care if you show up every day so they get paid. Buprenorphine? It’s a marketing ploy by Indivior to sell more Suboxone. The ‘ceiling effect’ is a lie-there’s no ceiling. They just don’t want you to take more because then you’d need less pills. It’s all profit.
And the ‘studies’? All funded by pharma. The 81.5% retention rate? That’s because they won’t let you leave. You get kicked out if you miss a dose. That’s not treatment-that’s incarceration.
Real recovery is sobriety. Not pills. Not clinics. Not EKGs. Just clean. No drugs. Ever. Anything else is just slow suicide with a prescription.
Martyn Stuart
Responding to the comment above: Your perspective is rooted in trauma, not data. I get it. The system has failed many. But dismissing MAT as ‘control’ ignores the lives saved. People who would’ve died from overdose are now alive because of methadone. People who would’ve relapsed into homelessness are now parenting because of buprenorphine.
Yes, the system is flawed. Yes, profit motives exist. But the solution isn’t to abandon treatment-it’s to demand better. More funding. More training. More dignity.
Calling people ‘slow suicides’ because they’re on MAT? That’s not advocacy. That’s cruelty disguised as purity.